We welcome questions or feedback about the Anti-Racism & DEI Course Materials Project:
ar-dei-project@uw.edu
Category: Uncategorized
Guest Blog Series: Srilata Remala
Srilata Remala is a nurse, philanthropist and parent based in Seattle, WA. These questions were developed by the team at MPS CARE in Nursing to learn more about Ms. Remala’s unique perspective as a nurse of color and philanthropist, and to shed light on the important links between nursing education, training and health outcomes for communities of color, and of the crucial need for anti-racism efforts within those spaces.
To make a gift to the Anti-Racism in Nursing Excellence fund, click below:
As a nurse who graduated from nursing school in December, what specific instances of racism have you witnessed or experienced that highlight the need for Anti-Racism initiatives in nursing?
I graduated in December 2023. It was always hard to find allies in the program (I had two professors of color). I routinely watched as students of color were treated differently to my white counter parts. When people of color advocated for themselves, they were seen as loud, rude and disrespectful. Meanwhile I watched, as my fellow students who were white, insult professors, make crude jokes, and act inappropriately with barely even a slap on the wrist. As students of color, we were not given the space to make mistakes. If we missed anything it felt like there was a spotlight on us. The person who was given our deans award at the end of the program routinely was disrespectful, and made students feel uncomfortable. Meanwhile, we had students of color, working multiple jobs, taking care of their families, and still showing up getting straight As but were passed off for the award. It’s such a good example of structural racism in nursing school and how it is designed to make students of colors feel like they are not enough.
The structure of the nursing profession isn’t optimized for the success of immigrants or individuals who are the first in their families to pursue higher education. Nursing school like most academia is falls into the traditional degree patters or paper writing and theory reading. There is little to no support for people who are non-English speakers. The NCLEX is not offered in other languages other than French, not even Spanish, because it prioritizes nurses who are fluent in English.
What are some key challenges in combating racism in nursing, and how do you see your contribution helping to overcome these challenges?
This is a very bold question, and I don’t have all the answers by any means but here are just a few of my thoughts based on my recent experience as a nurse:
- Barriers to entry are so high. I was rejected from 4 nursing schools. My undergraduate GPA was terrible, but I had a 3.9 on my science pre-requisites and a master’s degree. None of that mattered. They only looked at my undergrad degree as a predictor of success. A degree I recived when I was 18 years old.
- Pay professors and preceptors better. Part of the vicious cycle in understaffing in nursing is the lack of professors, poor pay, and lack of preceptors. The professors of color in my program both worked two jobs. They would support us during 12-hour clinicals, and the next day go work a 12-hour clinical themselves. Sometimes even multiple shifts
- We need to diversify. The American nursing association reported the current nursing workforce is “80.6% White/Caucasian; 6.7% African American; 7.2% Asian; 0.5% American Indian/Alaskan Native; 0.4 Native Hawaiian/Pacific Islander; 2.1% two or more races; and 2.5% other nurses. In addition, 5.6% of the RN workforce report their ethnicity as Hispanic”. (source). 80% white in a population where 40% of the people identify as people of color is not ok.
- Nursing students need to stop learning from old theories of nursing developed by people who perpetuated racism. There are SO many nurses of color, especially Black nurses, who have developed theories that are way more relevant to nursing today. I never learned about Harriet Tubman in nursing school-why was that?
- Enough with the DEI-related nurse courses or “health equity” courses. Let’s talk about health liberation and what that means to Black and Brown communities. A baseline of DEI should be taught during orientation. The purpose of nursing school should be to dive deeper. Where are the statistics worse for people of color? What conversations can we have as nurses that challenge the profession in hopes that outcomes are better for people of color?
- I work in a community health setting, and we often discuss how trauma, systemic oppression, and racism have contributed to poorer outcomes in Black and brown communities. As much as biological processes are important in understanding chronic conditions, there needs to be more of an emphasis and connection on the effects of systemic oppression on marginalized communities. A lot of patients fear the healthcare system understandably, as nurses it’s our job to ensure they feel safe and heard but to also acknowledge why they fear the system.
Can you share what motivated you to make a gift to support The Manning Price Spratlen Center for Anti-Racism and Equity in nursing?
The vision for the center was clear from the beginning and it was bold. Not many centers exist like The Manning Price Spratlen Center for Anti-Racism and Equity in nursing.
I personally was feeling defeated in my own experience of nursing school and felt like I needed to contribute back to make a change. Our family values education and we recognize the barriers in academia that prevent students of color from achieving degrees. Systemic oppression has created race gaps in education and inadvertently limited opportunities to succeed for students of color. We hope to be able to support students of color in their nursing journeys indefinitely by setting up this endowment. It’s a small drop in a large bucket and I hope more nurses continue to give back in ways they find meaningful.
How do you believe funding anti-racism efforts in nursing can positively impact outcomes for patients and the nurses who care for them?
Studies have shown that when people of color are served by nurses of color, the outcomes are significantly better. Funding anti-racism work helps nurses move towards health liberation for our patient by putting resources where it’s needed. Funding anti-racism work in nursing is critical to the longevity of the field. We are seeing nurses leave in numbers, high burnout and job dissatisfaction. I know so many nurses who were vocal about racist experiences either for themselves or one of their patients experienced, and instead of the institution fixing the situation, the nurse was reprimanded. This has to stop and I think the only way to make it stop is by continuing to fund efforts such as research, to continually identify and quantify the effects racism and biases have on our overall health.
As a nurse yourself, what advice would you give to others who are passionate about addressing racism in healthcare but may not know how to get involved?
Nurses have tried to speak out against racism within large intuitions. It can be held against them in many ways, in the form of hiring, public perception, and just overall self-esteem. Nurses need to band together better to combat racism. We all know that racism is a problem in healthcare, and we are most powerful in numbers as shown by the unions we have created. I think nurses have the power to transform healthcare in a way that has not been done before.
A dear friend of mine is currently a float ICU nurse in pediatrics. She is a mentor and an incredible advocate for kids and families of color. She’s been a nurse for 20+ years and in that time, has committed to leadership positions within her union, writing letters and walking the picket lines, and supporting new nurses through agreeing to precept and educate. On her off days she volunteers her time for various committees that are addressing racism within the institution she works in and is committed to nursing in a way that I believe over time will make substantial change. I am so grateful to nurses like her because she knows the field needs to change and has devoted herself to trying to be a vector for change. She has use her power and privilege for change.
What do you hope readers will take away from your blog post about your journey and the importance of anti-racism efforts in nursing?
Nursing is a critical field. We are considered a lifeline in healthcare, and a key role that can help eliminate health disparities with proper training and care. I want people to understand that we still have lots of work to do, and there is still so much change that needs to happen.
We are an immigrant family; my sister is the only one that has graduated from UW MPA. We have set up 3 endowments at UW because we are really committed to success of students of color. If we as an immigrant family with deep ties in India continue to invest in our community and in ending the barriers related to systemic oppression in the United States, then what is holding other people back?
How do you see the role of education and advocacy intersecting in the fight against racism in nursing? How can individuals act in support?
When people say they have experienced racism, believe them. When patients say they are uncomfortable or scared, help them and be their voice.
Harriet Tubman said “Every great dream begins with a dreamer. Always remember, you have within you the strength, the patience, and the passion to reach for the stars, to change the world.” I think its important for every nurse to have the self-confidence and belief that existing in this profession can change the world for someone. As nurses, we hold so much power in change, to speak out when things aren’t ok, and to support patients in their journey of health. All nurses matter and all nurses should feel empowered to have a voice.
Scholar Feature: Dr. Gina Higginbottom, MBE on Improving Health Outcomes in Black, Asian & Ethnic Minority Newborns through Neonatal Health Assessment Review

The Manning Price Spratlen Center for Anti-Racism and Equity in Nursing (MPS CARE) is featuring the groundbreaking work of Dr. Gina Higginbottom, MBE, Emeritus Professor Ethnicity & Health, University of Nottingham. She, along with colleagues Frankie Fair, Sheffield Hallam University, Amy Furness, Sheffield Hallam University, Sam Oddie, Bradford Teaching Hospitals NHS Foundation Trust, and Hora Soltani, Sheffield Hallam University compiled a report reviewing Neonatal Assessment and Practice in Black, Asian and Minority Ethnic Newborns. Their report examines the effectiveness of tests like Apgar Score, the Detection of Cyanosis, and Jaundice in black, Asian and ethnic-minority newborns and why these tests are less effective for these populations when compared to white newborns. We are excited to feature Dr. Higginbottom and this report on our blog as we know this work will contribute to the continued transformation of nursing practice and research, an endeavor which our Center is steadfastly committed to. Access the full report here: https://www.nhsrho.org/wp-content/uploads/2023/07/RHO-Neonatal-Assessment-Report.pdf
Continue reading to learn more about this work and Dr. Higginbottom’s perspectives.
MPS CARE: How can it be that infants have such disparate treatment?
Dr. Higginbottom: “Lack of clinical observational skills of in respect of infants with darker skin. The need for a national bank of images showing medical conditions in darker skin, improved training for healthcare professionals and the use of more culturally appropriate terminology. In respect of neonatal jaundice: Health professionals need to check for yellowing on the palms of the hands or the soles of the feet, which could be easier to see in babies with darker skin tones. Checking for yellowing of the whites of the eyes (sclera) and of the gums should also be used. These methods still rely on clinical observational skills which may be subjective, bilirubinometers provide a more objective measure.”
MPS CARE: What recommendations do you have to improve care for infants and pregnant people?
Dr. Higginbottom: “Our top three recommendations are as follows:
Area of Focus |
Who is it aimed at? |
| Policy | |
| Recommendation 3, page 151
There is an urgent need for regular education and training for healthcare professionals and healthcare students on undertaking clinical assessments on neonates from Black, Asian, or minority ethnic backgrounds, including within the yearly updates on neonatal resuscitation. Better education for families is also required. All training requires process evaluation to ensure effectiveness. |
Professional associations (including BAPM, iHV, NNA, RCOG, RCPCH,
RCM, RCN) and regulatory bodies (NMC and GMC) HEIs NHS Trusts
|
| Practice | |
| Recommendation 4, page 152
Guidelines that refer to neonatal assessment by skin colour should be immediately reviewed and updated to highlight the impact of race and ethnicity (BAPM, HEE, iHV, NICE, NNA, OHID, RCM, RCN, RCOG, RCPCH, Resuscitation Council, WHO). This should include guidelines around general care of the newborn, as well as specifically for jaundice, cyanosis and Apgar scoring. |
BAPM, HEE, iHV, NICE, NNA, OHID, RCM, RCN, RCOG, RCPCH,
Resuscitation Council, WHO |
| Research | |
| Recommendation 1, page 151
Jaundice: Exploration of wider availability and use of bilirubinometers is recommended to decrease health inequalities and ensure safe care for all. Collaboration with organisations such as CQC, RCOG, BAPM, iHV, RCPCH and RCM and other key stakeholders is recommended. |
CQC
RCOG BAPM iHV RCPCH RCM RHO to launch Jaundice ITT |
See report for additional recommendations.”
***************
Access the following articles to learn more about this work:
- https://www.theguardian.com/society/2023/jul/12/tests-to-assess-newborns-health-not-effective-for-bame-babies-in-uk
- https://www.mirror.co.uk/news/uk-news/calls-change-newborn-health-checks-30452218
- https://news.sky.com/story/newborn-babies-from-black-asian-and-ethnically-diverse-communities-could-be-at-risk-due-to-decades-old-skin-colour-test-12919467
- https://www.voice-online.co.uk/news/uk-news/2023/07/12/new-assessments-for-black-newborns-are-needed-says-independent-nhs-body/
- https://www.independent.co.uk/news/uk/asian-nhs-sheffield-hallam-university-b2373601.html
Access the full report here:
Student Blog Series: Lei Marshall
This week we are featuring an essay written by Lei Marshall. Read more about Lei, and her essay titled “Lōkahi – Balance” below.
 Aloha,
Aloha,
My name is Leionaona (Lei) Marshall and I am from Wai‘anae, Hawai‘i. I graduated from Central Washington University with my Bachelors of Science in Biology and am currently in the Accelerated Nursing Program and will graduate this summer. I plan to work as a pediatric nurse and eventually return home to Hawai‘i to serve my own community.
For most of my life, I struggled with my Native Hawaiian identity and establishing a meaningful connection with my culture. Unaware of the profound impact of colonialism and historical trauma, I failed to comprehend how these forces affected my understanding of my own identity, and the impact it had on the identities and connections of countless other indigenous communities. As I continue my journey of rediscovery, learning, and reclaiming my own sense of self, I hope to empower and amplify the voices of other indigenous individuals and
communities. Regardless of where you are in your journey, I encourage you to embrace your own unique story, honor your history, and take pride in who you are, and the legacy passed down to you from your ancestors.
I am a proud mother, wife, daughter, sister, and Kanaka Maoli. Mahalo nui loa.
Lōkahi – Balance
By: Lei Marshall
Mauli Ola– health. What is it? Every person has a unique interpretation of health shaped by their personal experiences and, even more significantly, influenced by their cultural background. Yet cultural integration in healthcare is not often seen in Western medicine, which tends to adhere to standardized practices and protocols. According to the National Cancer Institute, Western medicine is defined as “a system in which medical doctors and other healthcare professionals treat symptoms and diseases using drugs, radiation, or surgery.” However, even though the United States spends the most money on healthcare globally, it also has the highest prevalence of adults with multiple chronic conditions, obesity, and one of the highest rates of suicide. There is a huge disconnect between health and culture in Western medicine, a disconnect that could potentially solve many problems we see today.
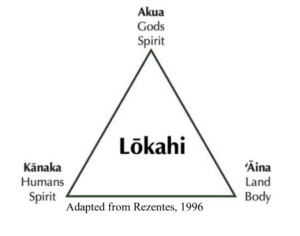
Before Western contact, indigenous communities had rich cultures and developed traditional practices and medicines. Tragically, a significant number of these traditions were suppressed or even banned as a result of colonization, depriving these communities of their ancestral knowledge and healing practices. Prior to Western contact, Native Hawaiian forms of healing/medicine included: lā‘au lapa‘au (herbal medicine), lomi lomi (massage), and ho‘oponopono (conflict resolution). These practices addressed the physical, psychological, and physiological aspects of health. In Native Hawaiian culture, health is a collective concept that extends beyond an individual level to family, community, the natural world, and the spiritual realm. They achieve health by following the Lōkahi (harmony/balance) triangle, which involves harmony between kānaka (humankind), ʻāina (land), and ke akua (god or gods). Illness or disease results when there is an imbalance, and restoring balance restores one’s health.
Cultural integration into health services requires incorporating both traditional and contemporary knowledge. Western medicine often prioritizes pharmacological or surgical interventions without considering incorporating cultural practices as an option before resulting to invasive treatments. Integrating cultural elements into a patient’s health management not only expands their range of treatment options but also empowers them with autonomy in selecting their preferred approach to treatment. This fosters a strong rapport and trust between healthcare providers and patients, enhancing the overall quality of care. A clinic located in O‘ahu conducted a study where they provided both Western medicine and Kānaka ‘Ōiwi (Native Hawaiian) healing practices, particularly lomi lomi. The findings revealed that 76% of patients believed that optimal healthcare could be achieved by combining Indigenous and Western treatments (Oneha
et al., 2023). Including culturally relevant interventions and integrating them into patients’ care is crucial as it addresses current symptoms and diseases and enhances patients’ health outcomes by fostering collaboration, respect, and a deeper connection to their health and culture. Minorities often face the label of noncompliance, but when we delve into the underlying reasons why patients may struggle to adhere to their treatment regimen, it frequently stems from a lack of cultural understanding and respect.
The consequences of colonization continue to affect indigenous communities leading to ongoing suffering from historical trauma. This has resulted in the loss of significant cultural traditions and practices, leaving families and communities grappling with the challenge of reclaiming their identity. In the face of these circumstances, incorporating culturally sensitive care into health services represents a modest yet meaningful step that the United States and Western medicine can take to facilitate the healing of trauma, foster the restoration of trust, and assist communities in reconnecting with their authentic selves. Integrating culture into Western medicine is more than just another means of treatment, it is staying connected through generations, optimizing health for not only yourself but your community and environment.
It is clear that the U.S. is a broken system—a system that prevents equitable access to culturally sensitive care. Not only does the system fail to integrate cultural practices into Western medicine, but also fails to include indigenous communities in decision-making processes. Culture is appropriated, not appreciated. It is time we remember the intrinsic value of cultural diversity and the profound impact it has on individual and community well-being. In doing so, we can begin to rectify the injustices of the past and shape a more compassionate future. By actively listening to indigenous voices, respecting their knowledge systems, and co-creating healthcare solutions, we can honor their resilience and wisdom.
References
Oneha, M. F., Spencer, M., Bright, L., Elkin, L., Wong, D., & Sakurai, M. (2023). Ho’oilina
Pono A’e: Integrating Native Hawaiian Healing to Create a Just Legacy for the Next
Generation. Hawai’i journal of health & social welfare, 82(3), 72–77.
Oshiro, K. H. Office of Hawaiian Affairs, Research Division, Demography. (2015). Native
Hawaiian Health Fact Sheet 2015. Volume III: Social Determinants of Health. Honolulu, HI.
Student Blog Series: Ben Evans
This week we are featuring an essay written by Ben Evans. Read more about Ben, and his essay titled “Social Praxis in Four Acts” below.

Ben is a current student in the Accelerated Bachelor of Science in Nursing program at UW Seattle. He was born and raised in Hong Kong before going to Macalester College for a bachelor’s degree in Urban Geography. After Macalester, he lived and worked in Santiago, Chile for three years and became a certificated K-12 teacher. He then settled into a 20+ year career in public education in the Seattle area, driven by the pursuit of educational justice and antiracism. These same values drive his desire to confront inequity and seek social justice in healthcare.
Social Praxis in Four Acts
By: Ben Evans
Act I: The Quandary
Nurses form a critical mass of individuals in healthcare who together can make massive impacts on the healthcare system as a whole. For this reason, they often find themselves center stage with their unique perspective and understanding of complex social issues. Their voices can be powerful in swaying public opinion and understanding. Nurses have, and always will be, the nexus between the medical world and our communities. They can be agents for change, or complicit in the rehearsed routines of the status quo. My hope for nursing is that we take responsibility to be the agents for positive change.
Responsibility for change is critical in institutions that prepare new nurses to enter the workforce. New nurses are representatives of the latest research and the most current understanding of nursing roles and responsibilities in healthcare. New nurses are at the peak of their holistic understanding of the profession, having recently completed classes and clinical experiences in a variety of health care settings. They can bring perspectives and ideas into the workforce that are transformative. Thus, how we prepare those nurses has a profound impact on the entire system.
One of the most important points of preparations is the role we play in health equity and antiracism work. The conversations around antiracism and health equity, while ostensibly ongoing, are functionally absent in much of the broader healthcare profession. At universities, where the most progressive thinking is happening, many faculty appear uncomfortable engaging in meaningfully pervasive antiracism work. Instead choosing to compartmentalize antiracism into units, lessons, or an add-on slide in their slide deck. Their stage fright to engage has profound impacts on the new nurse’s ability to confront these issues as they enter their professional practice. We need to step up our ability to navigate our spaces and elevate our comfort level to engage and think critically about the roles we play in systems of racism.
How do we take the profession of nursing and empower nurses to be the agents of this change? Protagonists that can move the needle on racism in healthcare. First, we need understand the barriers to the dialogue. Some believe the primary limitation is in language. Much of the equity training I have participated in revolves around this idea. By learning the right words and phrases we will have the tools to have the big conversations: equity, cultural humility; microaggressions; white privilege; decolonization; diversity and inclusion. While this is important, it is like saying the key to successful surgery is learning to wash your hands. Importance doesn’t change the fact that it is just a line in a whole play.
The overarching theme that puts a halt to deepening our communal discourse is the pervasive centering of whiteness in almost all aspects of healthcare. While right in front of us, it is invisible to most people – cloaked in “plain science” and “fundamental concepts.” If we can dethrone whiteness as the central perspective in our training, resources, and conversations we will begin making huge strides in health equity.
Act II: Decentering Whiteness
As with any ailment in healthcare, we are on the lookout for indicators of improvement. If a patient has an infection, we watch for their temperature to go down. When we know systemic racism is rampant, what is the indicator that will tell us we have found a treatment that works? Amidst the performative, equity-word-salads of healthcare mission statements, speeches, and promotional videos, the red herrings are abundant, but one true indicator of our progress on health equity is when we see a shift in the de-centering of whiteness. To many BIPOC nurses, this is a no-brainer, but for most healthcare professionals, centering whiteness feels more like “pure science.” Decentering the white experience is seen as an extra step to placate BIPOC sensitivities rather than an objective goal. So, what is the treatment for decentering whiteness?
Let’s look at why BIPOC Americans generally have a greater depth of knowledge and clearer lexicon when talking about racism. Is it really because they experience racism every day? Or is it something else? My mother is a first-generation Chinese immigrant and if you asked her if she experiences racism, she would say, “No.” Of course, I know this isn’t true, because I have seen countless instances of racism against my mother. So why then does she not see it as such? I believe it is less about the experience of racism and more a function of the discourse within her community. My mother has always surrounded herself with mostly conservative, white people, so the topic of racism rarely comes up. As a result, despite a multitude of experiences of racism, she remains entirely unaware of it, rationalizing that other people are ignorant, stupid or simply have “bad manners.” Her experience of racism doesn’t mean she knows more about it. Being a victim of harm does not always equal understanding what has happened.
Being a biracial American, I straddle two worlds between my white friends and family and my BIPOC friends and family. While my white friends are talking about the latest Indy-rock band they love or refinancing their mortgage for a cool home improvement project, the conversations I have with my BIPOC friends invariably have race intertwined into them. This disparity is the heart of decentering whiteness: not our personal experience of racism, but our experience in discourse and study of the dynamics of racism. If we can elevate the discourse on antiracism in our respective units, hospitals, social circles, and communities, decentering whiteness will happen as a natural consequence, an indicator. But how do we do that? Enter, Social Praxis.
Act III: What is Social Praxis?
As a teacher, I studied Paulo Freire’s concept of praxis – the point at which pedagogical theory and practice intersect. It was such a simple idea. Freire argued that educational theorists spent a lot of time patting each other on the back for being so clever, but until their theories intersected with the actual practices of educators, they were worthless. So, the goal of theorists should be praxis – absent of action, your words mean nothing. This is all fine and well, but how does praxis help us elevate our discourse on racism in healthcare?
Several years ago, I was thinking about praxis while talking with some BIPOC colleagues and collaborators about the efficacy of an in-service training on equity in education. I held the viewpoint that the trainings are useless in the absence of regular and consistent conversation about these issues in every aspect of our jobs. I started using the phrase, social praxis to describe the state in which complex intellectual concepts are embedded into social fabric. Embedded to such an extent that baseline understanding is high enough to begin problem solving instead of spending hours reaching consensus on definitions or even the existence of that problem.
In-service trainings can normalize and mainstream the big ideas and catch-phrases of an issue, but that is a far cry from embedding into the social fabric. Black Lives Matter signs are normalized all over Seattle, but that doesn’t mean people really understand what it is or its implications. BLM taught many Americans more about racism, but it has a long way to go before becoming embedded as part of our broader social fabric.
On a Saturday night during grad school, I went to two very different parties. One of my roommates threw a house party where all but one guest was white. I stayed long enough to hear a conversation between a large group of guests. The host’s boyfriend was explaining how, at 32 years old, he barely has to work because he just bought his second small apartment building and he finally turned it over to a management company. He was telling everyone how he pulled off this feat and everyone had questions. They were taking mental notes. All the participants were engaged and stimulated. They wanted to know the answers to their questions, scheming in situ to make their own real estate empires. Their baseline knowledge went beyond vocabulary and they were able to envision how these concepts could be applied to their own lives. This conversation had entered their social praxis.
From there, I drove across town to another party where there were no white people at all. I was the only Asian guy there, and everyone else was Black, Pacific Islander, or Latinx. Aside from the racial demographics, the guests were very similar to the first party. Most were college graduates, many with advanced degrees and solid income. There were some similar conversations, but the part that jumped out at me was that a huge percentage of airtime was taken up with discourse around race and identity. We dissected and delved into the racism we encountered that week at work, on the news, online, in the grocery store, and at school. Yes, we had experienced racism, but more than those experiences, we asked questions, analyzed, and applied each other’s experience to our own lives and understanding. The social praxis of race was so well developed that there was communal understanding at every level of the conversation. With the same level of engagement and stimulation as the first party, we were developing our understanding of race and racism in our communities and between different groups. We didn’t have to review jargon or confirm that racism existed. We just processed and exchanged our stories in community with one another.
This is our cue! This level of social praxis is what we need to stimulate real change in healthcare. Until the topic of racism enters this level of social praxis within a community, we cannot truly be able to understand and dismantle it together. How do we stimulate the social praxis of racial dialogue in nursing? How do we insert it into the psyche of nurses so that they want to talk about it at parties?
Act IV: How do we build social praxis in nursing?
In his book, Outliers, Malcolm Gladwell postulates that we need 10,000 hours of practice to reach a professional level of functioning in anything we choose. 10,000 hours of understanding racism doesn’t happen with a yearly in-service training, a slide in the PowerPoint slide deck, or a one-off lecture in week six of your nursing school program. We can’t simply use one-off solutions and quick fixes. Weaving the fabric of social praxis starts with talking about racism and equity every day. There must be a multitude of solutions that are subjective, individualized, community-minded, and ongoing. They come on many levels and in many forms, but all should be aimed at developing the social praxis of antiracism work.
In nursing education programs, thoughtful integration of antiracism discourse should be happening in all aspects of program implementation. It starts from admissions and orientation, then continues through organizing schedules, planning faculty retreats, class activities, social events, advising, and eventually, resume building workshops, and job searches. Antiracism work must be built in seamlessly and ubiquitously.
Programs can support events that provide spaces for thinking outside of the box. In March 2021 the UWSoN held the “Antiracism Learning Day” – a potential catalyst to synthesizing social praxis around race. Unfortunately, this was a one-off event but along the right lines. It was an attempt at making a space that could engage us and give us a place to talk about race. Where everyone can meet to be on the same page. Events or experiences like this should give us no option but to want to talk about race when we see our friends and colleagues.
As individuals we have a responsibility to push for this work. We can choose where to begin and how much energy we can spare, but we have to start it. We can develop our own professional communities that grow the social praxis of racial discourse, talking about it often and holding each other accountable. We can speak up in classes or in discussion group. We can organize events and facilitate critical thinking exercises. Bring it up at parties. Talk about it with your friends. Ask about it at staff meetings. Whatever we choose, we must find our own place to begin and then get to work.
With the common goal of achieving social praxis of antiracism work, I believe we can make huge strides not only in working toward health equity, but also in elevating our communities toward deeper understanding of how we each participate in systems of oppression. The antiracism revolution in healthcare starts with finding our place in building the virality of racial discourse. At every turn, weaving antiracism work into what we do and say. When we embed it into the fabric of our work, engaged and stimulated, dissecting, dialoguing, scheming, and applying what we learn, then we can reach social praxis of antiracism in healthcare. That is when real change will happen.
Dispatches from the Interim Director
Dispatches from the Interim Director: Understanding Leadership Transitions
07 September 2023
Dear Campus Community:
First, as I reflect on my first year as a member of the faculty at the University of Washington, I appreciate your grace, your patience, and your support during my transition. Second, I write to you today to provide you some clarity and updates on my new roles and how to get questions answered. Third, please know you can reach out to me using the following email addresses:
| Title | Website | |
| Associate Dean (Interim) | sondei@uw.edu | Office of Equity, Diversity, and Inclusion) |
| Center Director (Interim) | carn@uw.edu | MPS CARE in Nursing |
| Faculty (please note mclemore is not me) | mclemor@uw.edu |
You can also find me @mclemoremr on all social media channels.
Why Interim Roles?
As I have stated publicly, I believe all leadership roles should be rotated, which is why I accept interim positions. This allows for flexibility in ideas, acclimating people with change, and nimbleness in decision-making. Interim roles have no bearing on my commitment to the work or the stability of the school! In fact, just the opposite, by stabilizing the roles of Center Director and Associate Dean, the permanent occupant(s) of those roles should have a solid foundation from which to build during their tenure.
What Should We Expect?
I plan to participate in all activities that Dr. Butch de Castro participated in – specific to new student orientation, existing meetings, student reporting (including bias reporting), as well as department and school wide meetings, particularly the DEI committee and student groups. I will also be rolling out new programming, expanding faculty development, and improving/streamlining bias reporting. A visual conceptualization of how we plan to complete our work for this academic year is below. When in doubt, if you have questions, just send an email.
What are Immediate Actions?
- Update Office of DEI website
- Develop Social media channels and develop an audience.
- Share roadmap from EDI RETREAT (scheduled on 8/7/2023)
- Acquire an office space and host ribbon cutting/barn raising for the MPS CARE in Nursing
- Hiring of staff person
How Do I Provide Input and/or Feedback?
The Center has set up a consultation form, as well as a feedback form, so we can track requests and receive feedback about our work. Please use the form as often as you need to!
As always, we welcome your comments, feedback, questions and suggestions.
Monica R. McLemore RN, MPH, PhD (Dr/She/Her/Hers)
Professor, Child, Family and Population Health Department
Interim Director, Manning Price-Spratlen Center for Anti-Racism and Equity (MPS-CARE) in Nursing
Interim Associate Dean for Equity, Diversity, and Inclusion (AD/EDI)
University of Washington, School of Nursing
Adjunct Professor, Department of Health Systems and Population Health
University of Washington, School of Public Health
NEW! Student Blog Series
We are honored to use our digital platform to feature exceptional scholarly work from UW nursing students, focusing on topics centered around Anti-Racism and health equity. It is crucial that students’ voices are amplified in this space, as it disrupts the power structures within academia and nursing that, historically, propped up the white supremacist status quo in both spaces. Equity is one of our core values, so we believe amplifying the voices of those with disproportionately less institutional power is one path toward equity in nursing and academia. We also strive to follow in the foot steps of our namesake, Dr. Lois Price Spratlen and Ms. Frankie Manning, both of whom were tireless advocates for nursing students, establishing scholarships, providing mentorship and support, to name a few things.
Dr. Ben Danielson Keynote Speech | UW SoN Convocation 2023

We were so moved by the words of Dr. Ben Danielson on June 9th 2023 where he gave the keynote speech for the School of Nursing Convocation. It is important, now more than ever, that our leaders take a stand and speak truth to power; we believe Dr. Ben Danielson (“Dr. Ben” as he is known among his patients) is a shining example of leadership with conviction. Benjamin Danielson is a pediatrician and clinical Professor of Pediatrics at the University of Washington School of Medicine. Danielson is known in the Seattle community for being an advocate and leader for underserved children and their families. Danielson has devoted his career to increasing access to healthcare and fighting against racial inequities. Throughout his time as a pediatrician, Danielson has facilitated the creation and development of diversity programs and contributed actively to governmental policy as a member of several health boards. Danielson was the medical director of the Odessa Brown Children’s Clinic from 1999 to 2020, where he then resigned and spoke out about prevalent institutional racism and a resistance to change from hospital leaders. In September of 2021, it was announced that Danielson would be directing a new program, Allies in Healthier Systems for Health & Abundance in Youth (AHSHAY) to help address and prevent youth incarceration. Dr. Ben was selected as the 2021 recipient of the Seattle-King County First Citizen Award.
We encourage you to read his powerful keynote speech below, or access the video, available here: UW School of Nursing Convocation 6.9.23 (vimeo.com)
Nursing Commencement Address 2023
‘This Quilt’
Ben Danielson
I wish I had all the right words to fully express, what an honor it is to share a bit of this time with you today. You are the truest and most skilled practitioners of the art of caring. You are the conscience and the devoted soul of this thing called healthcare. From the ORs, to hospital wards, to the labs, to the clinics, to our beloved communities. You are the first experience of warmth at the start of a patient’s care, the trusted constant during treatment, and the most supportive conclusion to the caring experience. You are the art and the soul of health sciences.
Art and Soul.
My regard for you is sincere and enduring. You were my first and best teachers. In my earliest and least certain days as a training physician, it was you who taught me, continue to teach me. In the highly technical realm of hospital wards, and – preciously to me – in the most soulful realm of a community clinic. You have, and continue to be, my brilliant teachers, my most patient guides. You’ve held out your hands and invited people like me to walk with you. To step where you step, traverse a path that I didn’t always see.
But you did. You, or someone like you, so very much like you, teaching someone like me.
So, yes, I’m incredibly honored to be in celebratory spirit with you today. And to say thank you, for what your ilk have already done for so many. And to say thank you, ahead of time, for what you will do for so, so many more.
I’m marinating in my own loving support of each of you, and I look around. I look around today and I realize my words of gratitude are just minor notes, compared to the roar of gratitude that fills this space; and rains down around us. In this joyous congregation of appreciation. This gathering is one more proof point, that this endeavor, this journey you’re on is, and always has been, a team sport. We’re all part of this trek.
Mutual aid in practice.
We see you. We see each other. I want you to know I see the network that makes this possible. You, the parent who poured every ounce of love into someone graduating today. You, the family member, the devoted friend who stood by someone here today; stood by someone who will traverse this stage. We see you, the person who lifted someone up when their spirits were low. And then did it again, and again, unselfishly. We see you, the person who believed in someone here, even when something had them not believing in themselves.
We see you, the peer, the training partner, setting aside your own pain, to ease someone else’s. We see you, the teacher, the mentor, the shepherd, encourager, always ready to help.
We see each other today, we take a moment to pause, to look around, to take this in.
To acknowledge each other, to share this energy. Share in the power of this moment; to be present and appreciated,
to be unmistakably present, right here, right now.
We also know there are more people here than can be seen. We know there are so many more who have been in your corner. In fact, there are people you’ve not met who are part of why you’re here today. There are ancestors in this house of gratitude today. There are ancestors with us today. There is more here than we can see with our eyes. Whatever makes up our selves, the patterns of our personas, our individual colorful and patterned patches, are woven together into a beautiful, glorious quilt. A quilt, whose warmth and tensile strength, helps us know that, even the patches that are far apart are connected. Even when we are far apart we’re still connected. Wherever our journey takes us, we don’t actually leave anyone behind. We are woven together in a quilt whose very nature reminds us we’re never alone.
This quilt…it travels back in time. It tells the story of nursing, the history of caring. This, the nursing profession, is – in a way – a story of us. Of our society, of our history; and it can foretell our future. It is a testament to the best of who we can be. And for every famed moniker of who we can be, for every name we remember, there are countless more shining souls, whose names aren’t recorded as often. For every Florence Nightingale, there is Mother Seacole. A Jamaican-born nurse who was not allowed, to serve in the Crimean War, like Nightingale did. Yet found so many ways to serve the ill and injured. From soldiers returning from war, to those suffering malaria. Served in ways just as deserving as Nightingale, of canonization. All of you, in your heart and soul work, will be doing magnificent things.
Whether it’s written into history or not, we still see you, and appreciate you for all you will do.
You’re still, forever, part of this same loving quilt.
You’re on an amazing journey. In our celebration of you wonderful graduates,
we take loving note of the legacy of nursing that is yours to claim. Claim your legacy, in this sacred space of healing. For you are healers, capable of healing even our deepest wounds.
Capable of raising your voices and bending your talents, toward healing our deepest wounds, individually and societally. Able to contend with our most heartbreaking concerns. Equipped to right our societies greatest wrongs. You are vested, with the honorable mantle of nursing.
You are imbued, with the talents of nurturing and healing. You are spirited, with the legacy of caring. These qualities make you the ideal champions for dignity and justice.
To me, you are the best hope for healthcare equity.
You bring to mind our legacy of champions for equity, dignity and justice. This art and soul, this moment, brings hope. Our ancestors are here, with us, in this sacred space. In this space we see, we honor, we recognize, we are lifted up by Harriet Tubman. Harriet Tubman: nurse, abolitionist, loving guide, conductor to freedom. Proactive treater of societal illness, civil war spy, champion for our better path. Nurturer of our better selves. Harriet Tubman: nurse, especially for civil war soldiers, formerly enslaved people and aging veterans. Tubman’s never-stop spirit is a legacy you are now part of. Her’s is the blazing honor that you inherit. The honor, and responsibility, to passionately speak out against injustice everywhere, while compassionately tending to the ill, anywhere. Your art and soul intermingle in this legacy now. This is now part of your diploma, this is part of the journey, this is part of your quilt. And so, I cherish you and look to your leadership, to guide us through the thick wood and tangling bog of healthcare injustice, on the trail to true equity.
There are countless shining souls in this space with us today. Some have been part of your lives; some have been part of mine. Liz Thomas is part of this space, part of our shared and glorious quilt. Liz Thomas, the University of Washington’s first African American, to graduate from its advanced practice nursing program. And the truest leader of the clinic I worked in.
Ms Thomas demonstrated, every day, that providing dignity is the best component, of the best kind of medicine.
And that dignity is the purest, most fundamental form of equity.
It might feel a little hard to talk about things like dignity and equity right now, especially in the last year or two. Our workforces are exhausted, feel under-appreciated. Time itself seems to tilt against our sense of peace and rejuvenation. Our systems of care are overwhelmed with the levee-breaking surges, of trauma and stress, with the reckonings of under-investments, in things like meaningful mental health services. Hard to talk about these things.
When we are harming each other, and ourselves, in the most tragic manners imaginable. It’s unimaginable, unimaginable, to me, as a pediatrician, to witness a time when the leading cause of death for children in this nation would be gun violence. And yet this is where our country is today. Something so preventable, so directly subject to our shared will.
So much in our control to change.
It is unimaginable to me that we, as a nation, are settling for this.
Well, I won’t settle for anything less than you. Because I’m convinced, that your spirit, your talents, your Tubman spirit, is needed now more than ever. Convinces me that, as champions for equity, you won’t allow these treatable woes, to hold sway. You will guide us on a better path. This is what equity is about. And champions for equity are needed now more than ever.
You are needed now more than ever.
It can feel hard to talk about equity right now, when the executive suites in our healthcare system, are mostly focused on buying each other up; are mostly trying to out-corporate each other. Trying to solve human problems with corporate solutions. It can feel hard…Yet I say to you again, that this is a time when we most need to focus on equity. Because equity is the path to humanizing our existence, our regard for each other. Your ability to cultivate and emanate dignity, the root of equity, helps us see ourselves as valued, caring people, who are worthy of being well cared for. A focus on equity, a fundamental emphasis on dignity,
is the root to rehumanizing healthcare, is the freedom map out of the situations we’ve come to think of as un-navigable, the solutions to the challenges we thought unsolvable.
This moment, this space, with this kind of history…Mother Seacole, Harriet Tubman, Liz Thomas, and so many more shining souls…This is your moment and you are exactly who you need to be. You cradle hope, you are the place where equity holds its greatest potential,
delivers on its greatest promise. And, perhaps, yes; you also hold great responsibility. Your work, your sacrifices, your brilliance, your very existence, has the greatest prospect to ensure a person seeking healthcare, a person otherwise rendered both invisible and, ironically, also harshly over-scrutinized, by this society, can know, thanks to you, that they are respectfully seen. A person ostracized in other spaces, because of their skin color or their abilities, or identities, or any other reason, can feel that they undeniably belong. A person regularly denigrated by poverty, can experience the richness of dignity.
You are the ones who carry that sacred duty. You’re the ones who will notice, when dignity and belonging are missing.
Yours is the profession that has taught, demonstrated, led and demanded, that all the rest of us in healthcare level-up, elevate our regard for dignity. Because there is no ‘care’ in healthcare when dignity is not present. And dignity won’t be found in a corporate playbook. Which is why you – as lighthouses of caring – are so important. So important, in fact, that you should never have to work in environs, that are un-sustaining or demeaning to you. You are wonderful people on a wondrous journey. A lot will be asked of you, you know that, you’ve known that from the start. A lot will be asked of you and, as giving as you are, you will be generous with your hearts and brilliance; well beyond the asking. All the more reason: you deserve to be treated with the greatest respect. Honored for your many gifts and immersed in a healthcare environment, where you are fulfilled and appreciated and justly rewarded.
All the more reason: people like me, who admire you so, should be doing more, a lot more, to help unbuild, deconstruct, tear down, the exhausting and sometimes morally hazardous aspects, of the healthcare system we have today.
It’s time. Time to reimagine this profession, fortify this avocation, and discover the kind of healthcare, that meets this moment in our history, and is worthy of you. You deserve to work in spaces that flow with affirmation, for how much your talents are cherished. Right now, when our healthcare system seems to teeter. Right now, when the future of healthcare hangs in the balance, and must be decided by channeling our best selves. And by calling on our ancestors.
It must be forged by your art and soul.
This quilt called nursing… it’s strong. This may be the very best time to be entering this field.
To answer the calling to become a nurse professional, right when the profession is calling for your voice. To be an influencer, a sculptor of healthcare’s future. And our future, our shared, covalently bound future, welcomes you. We all set our loving gaze upon you and we invite you to usher in, a humane, dignifying and heart-centered era of medicine. So, you see, we need you, each of you, more than any other time in healthcare. We need your wisdom, your compassion, your vigilance. And your ability to be a conscience for the rest of the healthcare family. You are in the position to see everything. From both the perspective of a patient,
and of a provider.
Your rightful place has been prepared for you by your ancestors. Every great nurse has been preparing for your time here. Every spark of brilliance in this profession is lighting your path.
Every nurse before you, the humbly unsung and the widely celebrated. They’re all here, for you. From the names I might know, like: Robin Hall, and Cynthia Brown and Happy Salinas-Santos, and all the cherished nurses I’ve worked beside. From all those nurses you might know; doing-what-they-do to nurture, and heal, and advance the humane journey,
across our communities, hospitals and labs today.
From the nurses whose names many don’t know…To the names we do know…To Harriet Tubman. With an ability only a nurse could have, to transcend enslavement, liberate bodies and souls, transect the Mason Dixon line and transport souls to freedom. Be the warrior for freedom and heal the wounds of others who also fought for liberation. Harriet Tubman, who’s very existence shamed the purveyors of kidnapping, and middle passages, and shackles and forced labor and cultural erasure. Whose power, audacity and ability to heal beyond humans, to heal humanity, could only come from a nurse. Harriet Tubman, who’s enduring spirit shames the worst parts of healthcare today. And glorifies the best of the caring professions… you. Harriet Tubman, who offers her unquenchable fire to you, to carry you forward, each step on your amazing journey to come. To lift you beyond one moment, one hard stretch, even one exhausting tenure.
This quilt called nursing is really beautiful. Known or unsung, every nurse before you is connected to you now. Offering you every one of their best lessons, sharing their love for this work with you. Holding you up higher than maybe you thought you could rise. And holding up hope that you will carry this caring profession a little further still. Hoping the best for you, hoping for your best. And watching all of us, to make sure we do right by you.
Imbue your days with the dignity you deserve. Harriet is watching over you, and she’s watching us too. To make sure we dream alongside you, follow your lead, give you your due, and to make sure we never take your caring for granted.
To make sure we honor your art and soul.
Antiracist Leadership Institute | Office of Minority Affairs & Diversity
School of Nursing Community,
The Office of Minority Affairs & Diversity (OMAD) is offering a wonderful training opportunity for leaders looking to hone their anti-racist leadership skills.
- Dates: Two days, July 26th 9 am – 3 pm & July 27th 9 am – 12:30 pm
- Lunch will be served on July 26th.
- Location: HUB 214
- accepting up to 30 participants for the institute.
- Please submit your intent to participate by June 23rd, 2023.
For more information on this 2-day training workshop, click here: Antiracist Leadership Institute – Office of Minority Affairs & Diversity (washington.edu)
We’re Hiring!
Hi SoN Community!
We are seeking graduate student writing assistants to help us write white papers, reports, and other materials this summer 2023!
This is a Part-time (10hrs./week) position, $25/hr.
See Handshake posting here: Writing Assistant | University of Washington – School of Nursing | Handshake (joinhandshake.com)